Purpose
To provide information on the mechanisms and physiology of transcranial magnetic stimulation (TMS), and its potential side effects.
Overview
Transcranial magnetic stimulation (TMS) is a safe, painless, non-invasive way of activating neurons in the cortex of the brain.
A plastic coil with an insulated coil of wire is held gently against the patient’s scalp. A brief current is passed through this insulated coil, which generates a brief and rapidly changing magnetic field around the coil. This magnetic field passes painlessly through the scalp and skull. The magnetic field is shallow, and can induce current flow in the underlying tissues. It can depolarize neurons near the surface of the brain causing them to fire in unison.
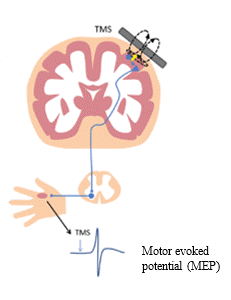
When the TMS coil is positioned over the primary motor cortex, the synchronized activation of neurons can generate a descending signal to the spinal cord and the alpha motor neurons that generate movement. This signal causes brief activation of muscles on the opposite side of the body which can using surface electromyography (EMG). TMS can therefore provide a safe way of testing whether the descending motor pathways from the brain to the spinal cord and out to the muscles are working. If a signal
There are various TMS protocols including single-pulse, paired pulse and repetitive TMS. VERIFY uses single-pulse TMS, where one stimuli is applied at a time and there is no cumulative effect. This protocol is used for assessment (not treatment) of the descending motor pathways, and is associated with the lowest risk of side effects.
The motor system
The motor system consists of the central and peripheral nervous system and the muscles of the body, with the motor cortex the highest level of sensorimotor control.
The motor cortex is divided into several distinct regions including the primary motor cortex, premotor cortex, the supplementary motor area and the cingulate motor area.
 If the TMS coil is positioned over the primary motor cortex which is located in the precentral gyrus of the frontal lobe the magnetic stimulus can depolarize pyramidal neurons that form the corticospinal tract. These pyramidal neurons are mainly found in layer 5 of the motor cortex, and are excited by intracortical interneurons located in the more superficial layers of the cortex, layers 1 – 4. Activation of these pyramidal neurons by TMS most likely occurs trans-synaptically via activation of intracortical interneurons, which in turn excite the pyramidal neurons.
If the TMS coil is positioned over the primary motor cortex which is located in the precentral gyrus of the frontal lobe the magnetic stimulus can depolarize pyramidal neurons that form the corticospinal tract. These pyramidal neurons are mainly found in layer 5 of the motor cortex, and are excited by intracortical interneurons located in the more superficial layers of the cortex, layers 1 – 4. Activation of these pyramidal neurons by TMS most likely occurs trans-synaptically via activation of intracortical interneurons, which in turn excite the pyramidal neurons.
When pyramidal neurons fire they generate synchronized descending output from the primary motor cortex to alpha motor neurons in the spinal cord, in the form of action potentials travelling along the corticospinal tract. When the descending output from the motor cortex activates alpha motor neurons in the spinal cord, they fire action potentials that then travel along the peripheral nerves to muscles on the opposite side of the body. Surface EMG can be used to detect the arrival of these action potentials in the muscles, observed as a motor evoked potential (MEP).
Obtaining MEP status for VERIFY
TMS equipment can be portable, so this means testing can be performed at a patient’s bedside, in a procedure room, or similar location. Depending on the patient’s level of impairment they may be in a chair, wheelchair, or bed during TMS for VERIFY. Family members can be present during testing, if this is what the patient wants. It will take up to an hour for VERIFY staff to set up, complete, and document the TMS assessment. The actual testing will take about 20 minutes for the patient although this can vary depending on the patient’s tolerance.
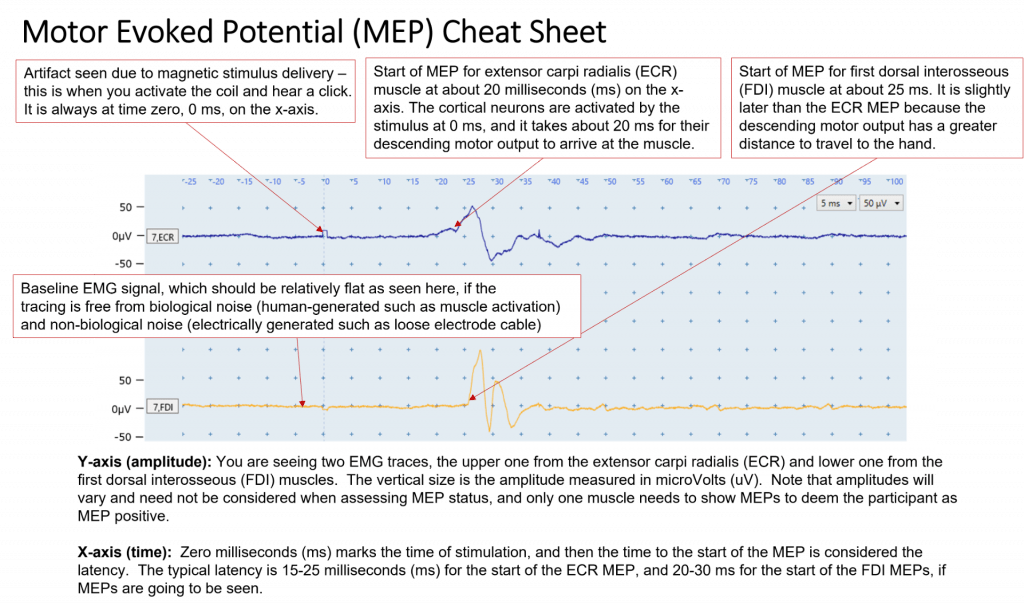
TMS in VERIFY is used to determine a stroke patient’s MEP status, which is whether MEPs can be elicited in either the extensor carpi radialis (ECR) and first dorsal interosseous (FDI) muscles of the upper limb in response to stimulation. MEP status is binary with two outcomes:
- If MEPs are able to be elicited it indicates descending signals from the primary motor cortex can reach the upper limb and the descending pathway from the primary motor cortex to the spinal cord is functionally intact. These patients are said to be MEP+.
- If no MEPs are able to be elicited it indicates the stroke has damaged the motor pathways and that descending signals from the primary motor cortex are unable to reach the upper limb. These patients are said to be MEP-.
The picture below will help orientate you to EMG traces and MEPs. The picture shows an EMG recording from the ECR and FDI muscles of the upper limb. In the picture below you can see a MEP is present in both the ECR and FDI muscles and so this patient would be classified as MEP+. A copy of the picture below can be downloaded from the here.
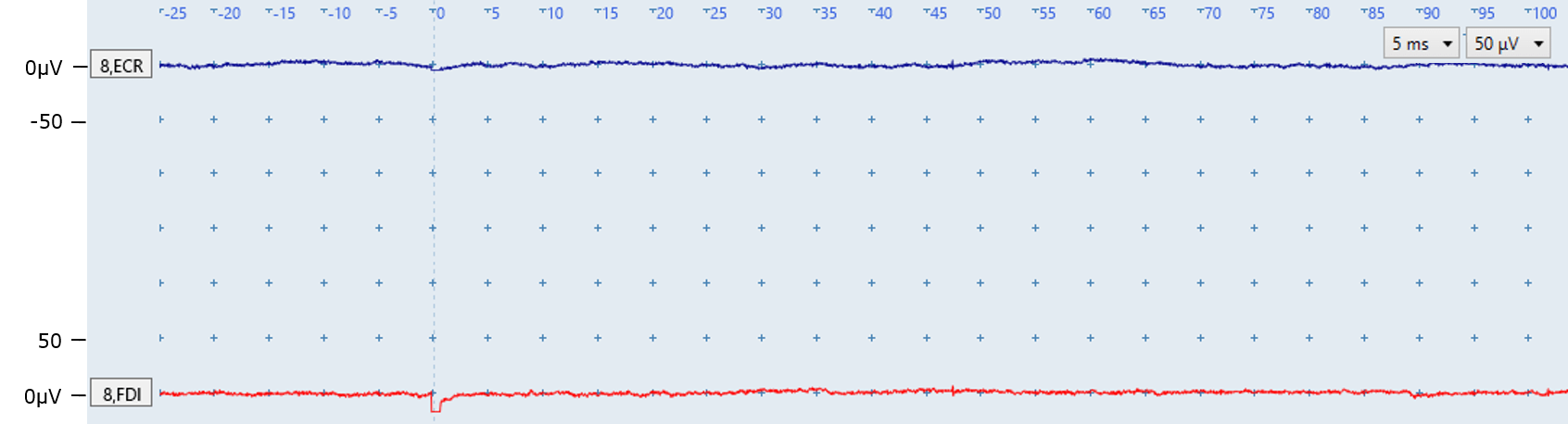
If TMS at maximum intensity is unable to elicit MEPs then the descending pathway from the primary motor cortex to the spinal cord is not functionally intact at the time of testing. In this case the MEP status of the patient is MEP-. In the picture below you can see an EMG trace from two muscles with no MEPs produced. If this picture was representative of all the EMG traces then the patient would be classified as MEP-.
TMS safety
Side effects are very uncommon, but it is important to be aware of them.
VERIFY participants must be screened for contraindications to TMS using the standard safety checklist. The next training module covers the safety checklist in detail.
Using this checklist minimizes the risk of potential side effects, which include:
- syncope – most likely due to anxiety rather than direct brain effects
- TMS-associated seizure activity – very rare for single-pulse TMS protocol such as the one used in VERIFY
TMS operators should be properly trained by personnel with expertise in TMS
Training includes theory and practical sessions. Operators must be familiar with the means for summoning medical or emergency assistance in their facility. If seizure or syncope are suspected during testing, TMS should be terminated immediately and first aid delivered.
People who are pregnant cannot be a TMS Operator for VERIFY but they can be the TMS assistant as long as the TMS coil is not activated within 3 feet of a pregnant person’s torso.
Further reading
Transcranial Magnetic Stimulation: A Primer
Resources
Frequently asked questions
Is it safe for everyone to have TMS?
The standard safety screening checklist must be completed before any VERIFY participant has TMS. Only a trained VERIFY staff member who has received a certificate for completing the TMS safety checklist module should use the checklist with VERIFY patients. The next training module covers the checklist in detail. A physician, physician’s assistant, or nurse practitioner who is part of the patient’s medical team is also contacted on the day of the TMS session to confirm testing is appropriate. In general, about 2% of patients are not suitable for TMS testing.
What does TMS feel like?
TMS is a comfortable experience for most people. Start by explaining to the patient what they can expect. This can include:
- that a plastic coil will be held against the side of the head to test the movement pathways from the brain to the hand and arm
- that the device makes a click noise each time it is activated
- they will feel a light tap on their scalp each time it is activated, but this won’t be painful
- they may or may not feel a brief twitch in their hand and arm muscles, but again this won’t be painful
- TMS is a well-established technique and is used all around the world in a wide variety of health conditions
How does single-pulse TMS differ from repetitive TMS?
VERIFY only uses single-pulse TMS.
Single-pulse TMS is where one stimulus is applied at a time, with several seconds between stimuli. When applied over the primary motor cortex single-pulse TMS is used to assess whether the motor pathways from the brain to the spinal cord are working. Single-pulse TMS has no long-term effects on cortical activity.
Repetitive TMS is where multiple stimuli are applied repeatedly, at a frequency of at least once per second. Repetitive TMS can change the activity of descending motor pathways for a period of time that outlasts the period of stimulation, often 30–60 minutes.
Put simply, single-pulse TMS can be used to investigate the function of the motor pathways but it does not modify their activity and does not provide a treatment effect.
Is single-pulse TMS like electroconvulsive therapy (ECT)?
Both ECT and TMS involve stimulation of the brain but their mechanisms, purpose, patient experience, and safety profile are very different. ECT is a psychiatric treatment that involves directing an electric current into a patient’s brain via electrodes applied to the scalp to intentionally cause a series of “generalized seizures”. Patients are given muscle relaxants and general anesthetic so they are not conscious during the treatment. Side effects such as memory loss are common.
By contrast TMS uses electromagnetic induction to non-invasively and painlessly activate cortical neurons. For TMS, patients are fully awake during testing and able to converse throughout the procedure. Single-pulse TMS as used in VERIFY is an assessment tool, and not a treatment, and does not induce a series of seizures. Side effects are uncommon, and tend to be mild and transient.
What should I do if a patient is due for TMS testing but their medical status has changed since I went through the TMS safety checklist with them?
Notify the person who is due to perform the TMS testing. The TMS Operator will need to review the situation and possibly revise the TMS Safety Checklist to reflect any changes. If the patient experiences a seizure between completing the checklist and TMS testing then they are now contraindicated for TMS and cannot continue in the study. A physician, physician’s assistant, or nurse practitioner who is part of the patient’s medical team should also be contacted on the day of the rescheduled session to check if testing is appropriate.
Survey and Quiz
The first of six quizzes you complete for the online VERIFY TMS Training should be for this TMS Overview module. A link to the practice quiz for the TMS Overview module will be sent to you once you take a short survey asking about your current TMS knowledge and experience prior to this online self-directed TMS training. The survey is not scored and all your answers will be anonymized.
If you score at least 70% in the practice quiz you will be emailed a link to the final TMS Overview quiz.
If you pass the final quiz with at least 80% correct you will be emailed a certificate of completion for the TMS Overview module. There is no limit to the number of attempts for the practice or final quiz.
Please email verify.study.tms@gmail.com if you have any questions or comments or require assistance.
